Health behaviours and levels of morbidity are key drivers for future mortality rates and can be thought of as key components of the “longevity pipeline”. The levels of health and morbidity in a population today will be stored up and reflected in how long people live in the future.
3 April 2019
In this edition of VitaMins Health we explore the subject of care homes.
Residential care can significantly prolong and improve the quality of life for individuals. But there are cases where the benefits are offset by the impact of moving into care or different routines. Significantly, the overall benefit derived from residential care appears closely linked with individuals’ socio-economic status.
While residential care can provide the much-needed support required by elderly people, it may appear surprising then that mortality and morbidity rates for people in care homes are worse than those living in the community. In fact, research shows age standardised mortality rates in residential homes to be 2.8 times those of community residents (and as high as 4.2 times in nursing homes). However, we need to take care when interpreting these results, remembering that care home residents are amongst the most frail and unwell in the population, many bringing with them pre-existing illnesses.
So, how should we interpret this information?
Those who are already unwell at the point of admission will inflate the statistics for mortality and morbidity rates in care homes. For example, the UK Malnutrition Task Force estimated that 37% of over 70 year olds admitted to care homes are already malnourished. However, certain conditions such as scabies and infections from antibiotic resistant bacteria seem to flourish in the closer proximity of people in residential care, although these closer proximities may well help residents deal with issues of social isolation and loneliness.
There is also evidence that the process of moving into a care home can be very stressful, contributing to higher rates of mortality in the early months after care home admission even after controlling for differences in demographics and health status.
Perhaps more worrying, however, is that there are treatable conditions found to be more prevalent in care homes than in the community. A study found that dehydration was more common in patients admitted to hospital from care homes than from their own homes. However, we note that the delivery of food and drink to those receiving care is a problem for both those in their own homes and in residential facilities: the Adult Social Care survey found that over a third of older people receiving care say they don’t get food and water when they want it.
What is driving these statistics
Reduced funding by local authorities is putting pressure on the quality of care being provided. Understaffing puts more strain on the staff members, meaning they can’t provide tailored care to each resident. Poor wages for care home workers results in a high turnover of staff. Staff turnover currently runs at 31% across all jobs in this sector, compared to a national average of around 15%. This high turnover can result in inconsistent care for residents as staff may not know residents well or understand their specific needs. Currently, approximately one in twenty UK social care workers come from the EEA, so should the UK leave the EU and pursue a low immigration policy, the gap in the social care workforce could reach over 750,000 by 2037. On the whole, underfunding of care leads to closures of homes, with 148 care homes closing in a single year (spanning 2017 and 2018). Additionally, demographic trends are anticipated to result in 50% more adults over the age of 85 by 2041. As a result, the strain on care does not seem likely to decline any time soon, with demand for care increasing rapidly.
What does Club Vita data show?
The Club Vita data set can give us some initial insights into Care Home mortality, although, we note that we cannot draw any definitive conclusions as our data is not specifically set up for these kinds of insights.
The below graph compares mortality rates as a proportion of the overall population for men aged 75 to 95. The data has been split into 3 socio-economic groups1 based on pension amount and postcode.
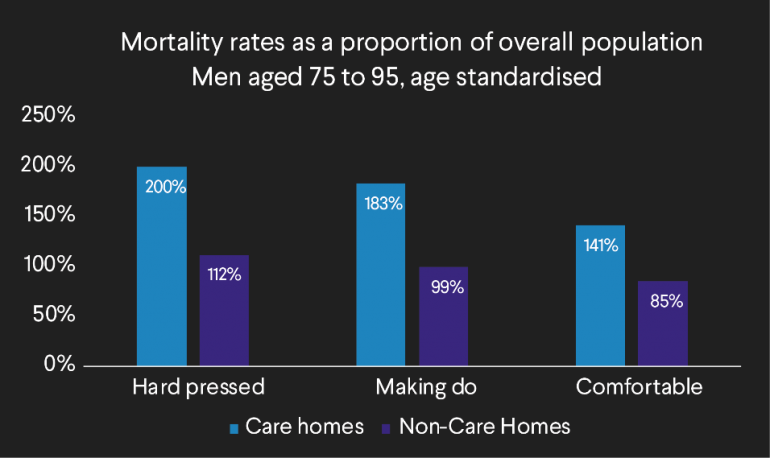
The data appears to show that there is some differentiation in the magnitude of excess mortality experienced in care homes across the socio-economic groups. Those in the Comfortable bracket, the most affluent, exhibit the least excess mortality. This could be due to a number of reasons:
- Comfortable pensioners are likely to be able to afford better quality care,
- Comfortable pensioners are likely to have more choice of care, or
- Comfortable pensioners may be less restricted in terms of when they enter care. Research by Bupa showed that those from more affluent backgrounds had longer lengths of stay in care homes. In particular, self-funded residents stayed around 35% longer than those with publicly supported funding. Deeming someone to require care can be a difficult decision for local authorities to make and time delays can mean the health status of pensioners has deteriorated further by the time of admission. Comfortable pensioners may therefore enter care homes in a better state of health than those in the hard-pressed or making do socio economic groups.
And what are the implications for pension schemes and insurers?
As the population ages, the demand for care is likely to increase and society will ultimately be judged on how it responds. Will we be able to increase the level and quality of formal care to meet the demand? Will we be able to find alternative solutions within society such as retirement villages or greater cross-generational care provision? Will we be able to increase the length of time people live in good health to reduce the need for formal care?
The effect on how long people live will ultimately depend on the answers to the questions above. And the effects may not be felt evenly across society. It will be as important as ever to monitor the emergence of any trends closely and how they apply to the specific populations of pension plans and insurance books.
What do you think? Please join the discussion in the Friends of Club Vita group on LinkedIn.
And don’t forget to follow Club Vita on Twitter and LinkedIn for regular longevity insights.
1 See our Longevity Trends report for definitions of these groups.
VitaMins Health: Care homes - the best place to grow old?
Download a print friendly version of this article.



